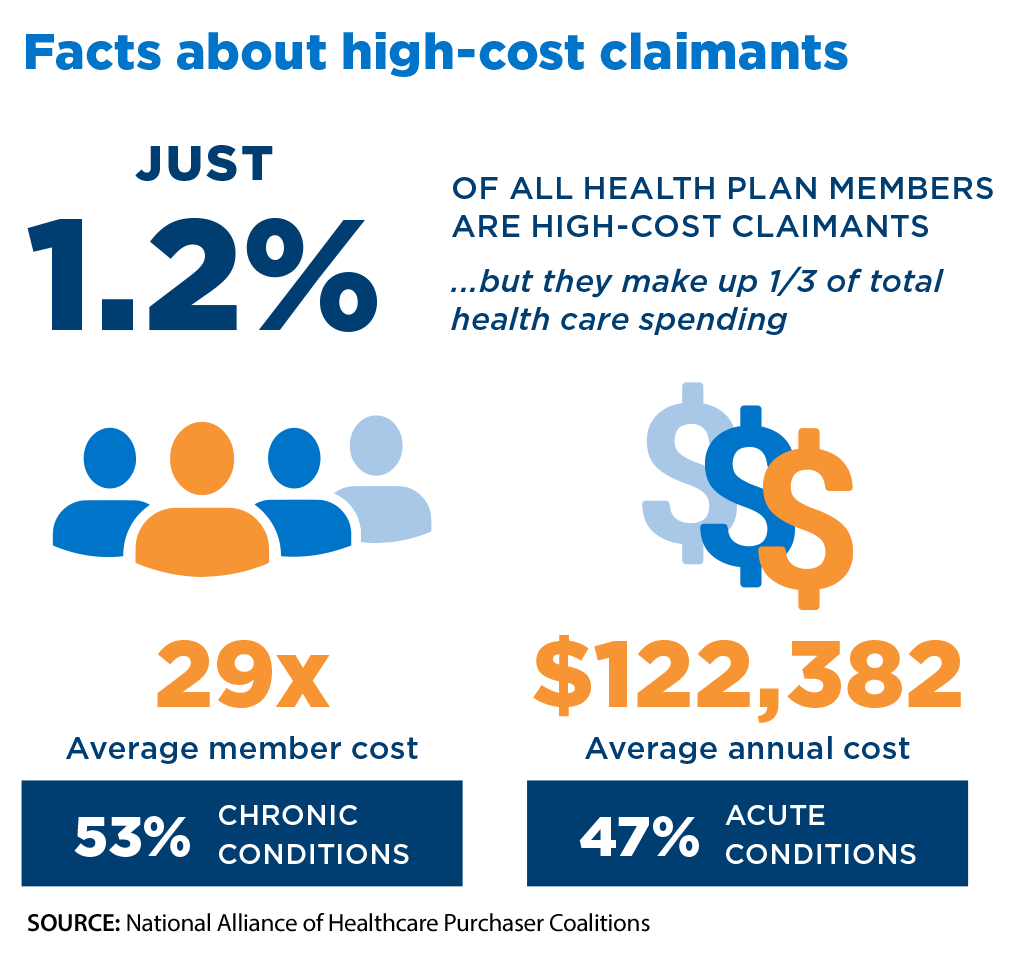
Million-plus dollar claims continue to increase… and not just from older plan members, according to a new report by the National Alliance of Healthcare Purchaser Coalitions (NAHPC).
“Employers are seeing a rise in high-cost claims for younger plan members, with $1 million+ claims disproportionately weighted toward this demographic,” the NAHPC report said. “The top conditions for these claims include cancer, prenatal/neonatal care, and treatment for COVID-19/long COVID.”
Among other survey findings:
- Since 2016, the number of health plan members with claims of $3 million or more has doubled.
- Nearly 8 in 10 employers consider drug prices, high-cost claims, and hospital prices a significant threat to the affordability of employer-provided health coverage for employees and their families.
- About 34% of employers set out-of-pocket maximums at $3,000 or below, while 42% have maximums of $3,000–$5,000. Almost 20% of employers have out-of-pocket maximums of $6,000 or more.
- Most employer strategies include a focus on managing complex cases (65%) and addressing the cost of specialty drugs (64%).
You can download the report from the NAHPC website.