A new survey on health and benefit strategies for 2025 finds that one-third of large employers will offer an “alternative medical plan” to steer employees to quality, cost-effective care. At MedBen, nearly half of our clients have implemented alternative reimbursement strategies that effectively balance top-notch care with cost savings and fair provider payment.
Among the strategies cited in the survey are narrow networks, in which health systems bill the plan at agreed-upon rates in exchange for exclusivity or preferred status. Through direct contracting, employers promote the use of quality care through local providers.
Here’s an example of how finding the right reimbursement balance pays dividends for employer, member, and provider alike. In 2022, a MedBen client contracted directly with three area health systems and offered a wrap-around PPO network for out-of-area care.
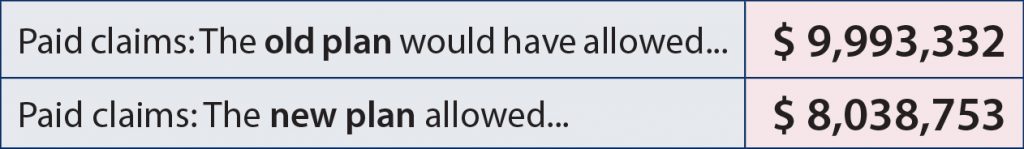
In the first 20 months, the client spent $1,954,579 less compared to their old plan – a 20.6% savings.
This is a “win-win-win.” A win for the member, who gets better benefits; a win for the provider, who gets a bigger market share; and a win for the employer, who gets greater savings.
MedBen can help you achieve the right balance through alternative reimbursement strategies… and we’re ready to show you exactly how we can do it. Just contact your broker or call us at 888-627-8683.