Want to take a deep dive into your 2024 plan performance? If so, there’s a great reporting tool you may not be using: MedBen Analytics.
Our online portal empowers you to make data-driven plan decisions through an employer dashboard, accompanied by a comprehensive reporting platform. While we offer over 100 customizable reports that you can download and review, below we highlight five of our most popular options.
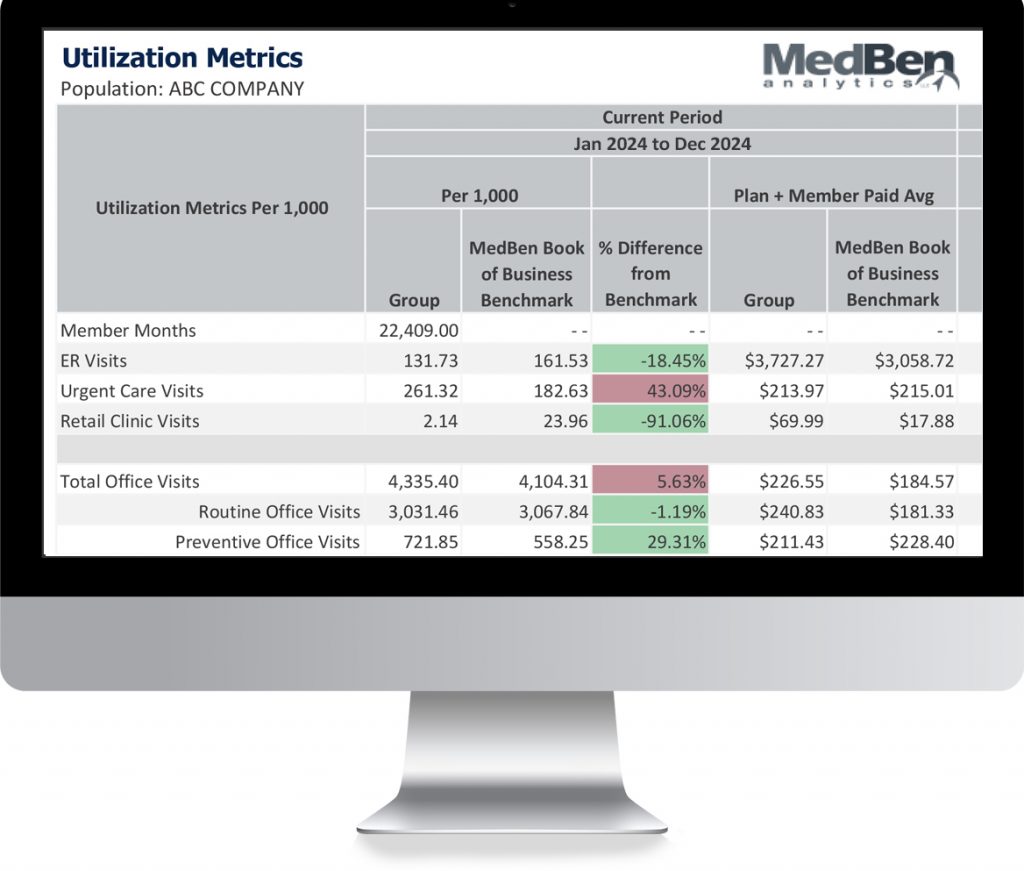
MedBen’s Utilization Metrics Report provides deep insights into how your members are accessing different medical services, with comparisons to previous periods and industry benchmarks to identify trends.
The Net Paid Claims Report tracks expenses that exceed your specified thresholds, enabling accurate projections of stop-loss reimbursements and helping you manage high-cost claims effectively.
The Health Plan Snapshot delivers an executive-level view of your plan’s performance, including membership and cost trends. This report helps identify key cost drivers and uncovers opportunities to optimize spend.
The ER Utilization Analysis identifies emergency room visits that could have been handled through more cost-effective care settings, helping you develop strategies to guide members toward appropriate care options.
The Medical IBNR Estimate Report provides detailed projections of incurred but not reported claims, organized by both incurred and paid lag months, supporting more accurate financial planning and reserving.
To generate these and other reports from MedBen Analytics’ Executive Analytics Portal:
- Sign on to the portal and select “Reports” from the left tool bar.
- Search and select the report(s) you want to view.
- Click the blue “Run.”
- Set your desired parameters and benchmarks.
- Click “Run” again.
- The report(s) will export as a PDF for you to view.
With MedBen Analytics reporting and the employer dashboard, you get actionable insights for better plan management. If you have any questions about using MedBen Analytics or haven’t yet signed up to use it, just contact your Account Management team.