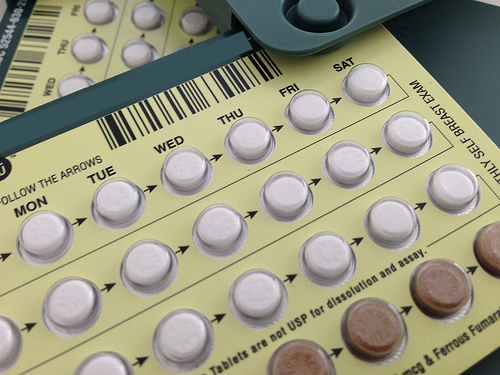
As you are likely aware, the Affordable Care Act (ACA) requires that all non-grandfathered group and individual health insurance plans provide access to FDA-approved contraceptives, including related contraceptive counseling and medical services, without cost-sharing through a preferred provider.
Although this requirement has been in effect for over a decade now, the Departments of Health and Human Services, Labor, and Treasury (collectively, the Departments) continue to receive complaints of plans being non-compliant nationwide. With the recent Supreme Court ruling overturning Roe v. Wade, the Departments will likely increase their focus on contraception coverage in the event of an audit in order to ensure ACA compliance.
As mentioned above, non-grandfathered group health plans must cover without cost-sharing at least one form of contraception in each FDA-identified contraceptive category, as well as related services that have been deemed medically appropriate by the attending provider. Reasonable medical management techniques are allowable under the ACA requirements.
Additionally, the Departments have strongly suggested that plans include a process for exceptions that is easily accessible, transparent, and sufficiently expedient, and that follows the attending provider’s recommendation for the individual receiving the contraceptive product and service.
If you have questions regarding your plan’s current coverage of contraception and related care, or if you believe your contraception benefits are out of compliance, please contact your Account Manager.